My paragard IUD insertion experience
If you told me three years ago that I would be getting an IUD at 21, I would have cringed and awkwardly laughed. I was content with my body and my health status. No need to get anything that wasn’t necessary. Although, now that I’ve got one and have been through the worst of the process, I don’t plan on looking back.
I was 19 years old when I first started using Tri-Sprintec, a combination pill for birth control. I’d taken a few months off from the pill since starting but was mostly consistent with it. Honestly, I thought it was how I’d avoid getting pregnant for the rest of my “fertile” life.
Now, there were times throughout that period of my life where I thought to myself, Do I really think I’ll be this consistent about medication in the long-term? Things got to the point where I had a hard time finding the perfect hour to take the pill every day. I’d either have to wake up early just so I could take the pill, or I’d already be halfway through my day and have forgotten to take it. Medicine began to feel like a chore.
I needed something I could rely on (that was highly effective) but also low maintenance without the side effects of hormonal birth control (in my experience, the pill had made me overly emotional, gained weight and raised my blood pressure to the point where I was concerned about my heart health).
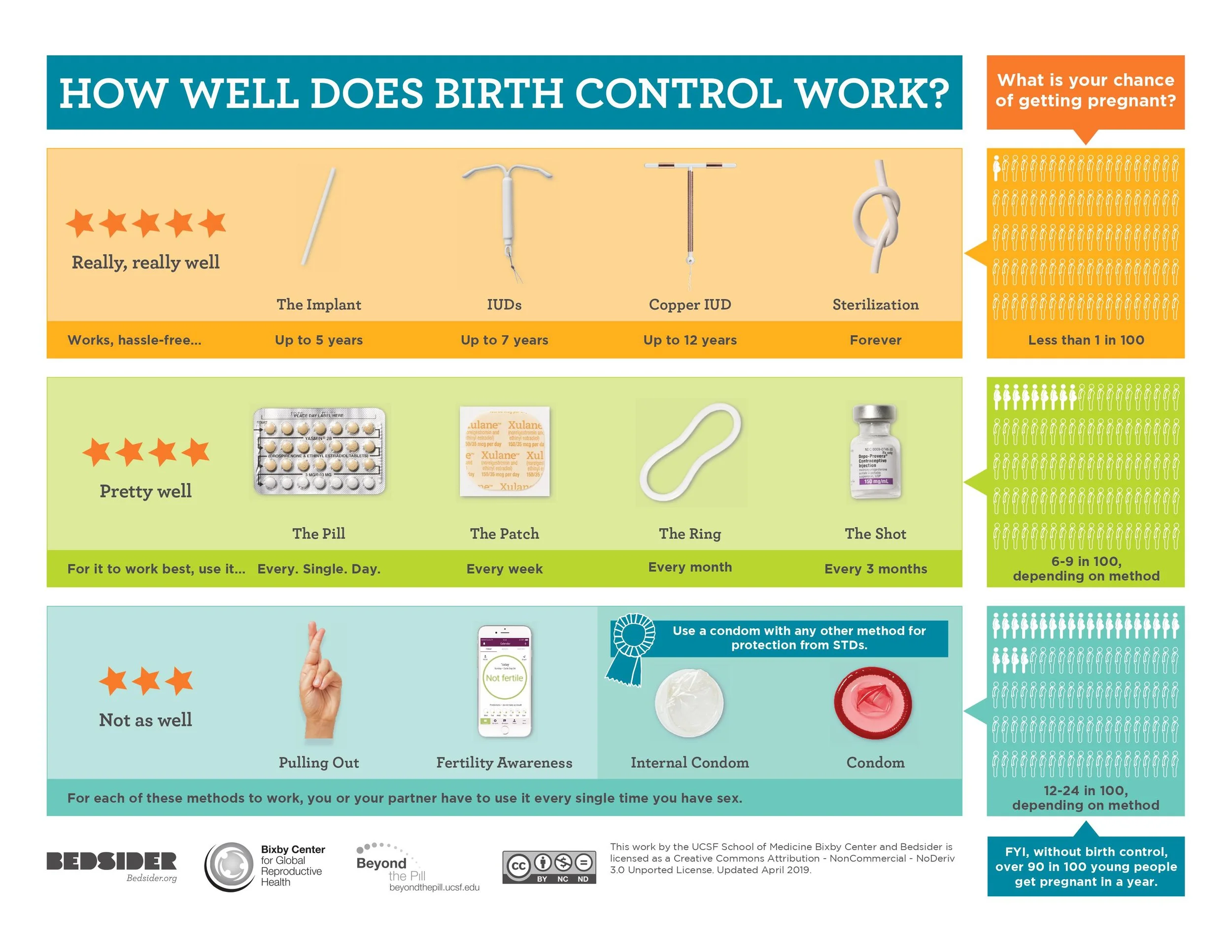
Doing my research, I found a common trend: The most effective contraceptive methods were hormonal. If you wanted to use a non-hormonal contraceptive, the efficacy was lower. This was unfortunate because I was most concerned about preventing blood clots, which is a possible adverse effect of all hormonal birth control. In combination with my blood pressure, I didn’t want to put myself at even more risk.
Then I came across Paragard, the only copper intrauterine device (IUD).
This option was the most attractive to me. Like other IUDs, this device is inserted into your cervix at the doctor’s office. It’s said to be 99% effective and has no hormones to affect my body’s natural levels. I also found it appealing that there’s a “set it and forget it” mentality that comes with IUD insertion and that this copper IUD lasts for at least a decade, in some cases up to 12 years.
Before officially deciding, I went to my primary care doctor for a wellness visit. We talked about my overall health including contraception. I told her I wanted to be proactive about long term solutions. I could tell she was making subtle pushes toward me getting an IUD or the Nexplanon. She showed me this chart and only talked about those rather than the full list of options:
I am really lucky to have a physician that agreed I should get an IUD especially because there are lots of haters out there. They avoid IUD-talk because they’re fearful of the pain, or there’s a negative stigma that’s associated (that you’re getting it to have sex) or that there’s something unnatural about getting a foreign device placed into your body (and seeing this as “bad”). However, she had no hesitations and encouraged me to think about my options before coming back.
A week or two after my visit, I officially set my insertion appointment. I also watched this video to mentally prepare myself. No matter what kind of IUD you get, the process is generally the same, and I’ll continue to explain it further later.
The morning of insertion day, the medical assistant suggested I take 600 mg worth of ibuprofen an hour before insertion, which is the most I’ve ever taken at once. I was nervous about the pain but more so excited I could say goodbye to pill-popping. That’s what I tried to focus on rather than potential complications that could come from this new device.
When I arrived at my clinic, a medical assistant took me to the exam room and showed me to a restroom to collect a urine sample (for a pregnancy test), and I was escorted into the procedure room.
When my doctor came in, she explained the whole procedure (if they don’t do this beforehand, ask them to talk through what they’re doing as they’re inserting down there if you think that can ease your nerves).
As every provider should, she also talked about possible risks. The main things were that my periods could be more painful and heavier for the first 3-6 months. She also mentioned to watch for heavy bleeding, or for possible IUD dislodging (which is another big fear that people have, however, this risk is extremely rare). With that, I signed the consent form and she had me lie down like I was getting a pap smear.
I’ve had a pap once, so the speculum insertion wasn’t that scary to me. I’m also a nursing student, so disinfecting the cervix (the highest point in the vagina) and spraying lidocaine (a topical anesthetic to numb the area) gave me security knowing I was getting cleaned and numbed. I was comfortable, able to talk and breathe naturally.
But then she inserted the tenaculum to clamp and pull the uterus straight. I felt excruciating pressure that I couldn’t relate to anything else, but I knew it was necessary so that my doctor could insert the uterine sound and measure the length of the highest point in my uterus to the end of my cervix. Even though it’s just a long, skinny metal rod with measurement markers, it felt like what I imagine a kidney stone would feel like (except in the vagina rather than the urethra).
I kept taking deep breaths through the pain, otherwise I would’ve probably started crying or passed out.
Once she had her measurements, she pulled the uterine sound out (which relieved some pressure, but the tenaculum was still clamped to my cervix, so I still felt some pinching). IUDs are inserted with their two “T” arms tucked into an applicator tube with more measurement labels on it. She inserted the tube all the way back up through the cervix and into the uterus, and once the IUD was in place, she could remove the applicator, and the IUD sat naturally in place.
Ouch. She told me I was a trooper through the whole process, but that was painful AF. She snipped the string of the IUD that hangs out into the vagina and lightly patted the area for some blood (which, in minimal-to-moderate amounts, is normal). She finally removed the speculum, and I could breathe normally again.
I still had residual soreness/pain near my cervix, so I stayed lying down for a couple minutes. My doctor (and her medical assistant) left me for a few minutes to get my Visit Summary while I changed from my hospital gown into my regular clothes. As I stood up and started moving around, I could feel my heart racing. “I really just got that done? Am I genuinely in pain, or just imagining it?” I put my dress and cardigan on fine, but as I leaned forward to tie my shoes, I felt my throat close, and nausea set in. I remember thinking, If I don’t move into a comfortable position now, I’m gonna yack. So I finished tying my second lace, lied back down on the procedure bed and closed my eyes.
As embarrassed as I was when the doctor walked back in, I was more relieved that she and her medical assistant gave me all the time I needed in the world to recover. In fact, I got a free apple juice and some crackers, which was probably the best part of the trip, before eventually getting up, waddling out of the doctor’s office and into the car to drive myself home.
To keep the rest of my story short, the cramping felt like constantly bad period cramps that wouldn’t resolve until my body got used to the foreign copper object. That didn’t last for more than two days, however, the bleeding/spotting lasted for roughly five days in my experience. I was allowed to take ibuprofen but stopped after the procedure day because I didn’t feel it was necessary.
It’s only been two and a half weeks, but as of now, I have no regrets.
Other pieces of advice I’d give?
If you have insurance, call the phone number on the card to make sure you know what is/isn’t covered. Most insurances should, but mine had conditions, like that my provider who inserted the IUD had to be “in network” to be a fully-covered procedure (I was lucky to find that my primary care physician was an in-network and qualified doctor to perform IUD insertions).
One thing I didn’t know before the insertion was that some doctors might recommend you don’t insert anything into your vagina for a week after the procedure, so that’s just something to keep in mind. That meant pads and panty liners for my bleeding, which isn’t the most comfortable, although I stuck with it because I was really worried about dislodging.
Be prepared for the pain and know what your pain threshold is. Take the pain meds. And, even if you’re nervous/not hungry before the appointment, eat enough that you won’t feel like passing out. I only had a banana and some water which might have been why I didn’t feel so well immediately after my insertion.
If you have a trusted friend/family member that can take you to and from the appointment, also ask if they can drive you, because it would have been nice to have had someone drive and be with me for a little bit after the procedure, in case anything were to go wrong.
For the pain after the procedure, a heat pack can relieve the discomfort, and it’s okay to take it easy for a couple days/don’t exert too many movements and stick to gentle exercise. Treat yo’ self to whatever you want to watch, eat, etc., use them as a staycation for you and your body to adjust. You’ll know when you’re feeling more ready to start trying out harder workouts or getting back to work if your job requires you to be active.
I’m still early into the journey, so I have a follow-up visit, periods and PIV sex to still encounter post-IUD insertion. However, as of now, I’m happy with what I’ve got and would tell anyone who’s thinking about birth control to consider getting one.
Photo Credit: Reproductive Health Supplied Coalition via Unsplash
This article was originally published on Parachute Media